FRIDAY, 27 APRIL 2012
It’s impossible to know when we made the connection between sex and conception. It has been suggested that the domestication of animals during the 10,000 years since the last ice age alerted us to our own biology, while the Bible speaks of Eve’s pregnancy after lying with Adam, indicating that it was well established by the time of the Old Testament.One thing seems certain: for as long as humans have known the secret of pregnancy we have tried to prevent it. While the cellular basis of conception, the sperm and egg, would not be understood until the Renaissance, history is rife with our attempts to prevent their union.
There is circumstantial evidence that population control occurred even in ancient times, with family sizes being lower than expected given the level of medicine at the time, but the Kahun Gynaecological Papyrus provides the first written proof. Dating to around 1800 BC, the Egyptian document is the oldest known medical text and describes several pessaries—barrier methods to prevent the entry of semen into the uterus. These concoctions frequently, and rather alarmingly, contained crocodile or elephant dung, but may actually have been quite effective by altering the pH of the vagina and killing sperm.
Although pessaries have been described by many cultures through the ages, they did not become commercially available until the 1880s, when London chemist Walter Rendell marketed a mixture of cocoa butter and quinine as a contraceptive. Although effective as an anti-malarial, quinine has since been shown to have no effect on pregnancy, and at high doses may actually cause renal damage in women. However, simply blocking the passage of sperm may have been sufficient to prevent many pregnancies, and early pessaries paved the way for modern spermicides and barrier methods, such as the diaphragm.
Despite these attempts to control conception, it may initially have been easier to terminate a pregnancy than to prevent it. The Roman chronicler Pliny the Elder wrote of the herb Silphion in his Historia Naturalis, which grew along a narrow coastline in what is now Libya. Though described as a contraceptive, it was taken monthly and so more likely acted as an abortifacient, or drug that induces abortion. Other plants of the Silphion family have since been shown to be high in the female hormone oestrogen, which is an active ingredient in some modern emergency contraceptives. There are occasional reports of herbs still being used where abortions are prohibited or difficult to obtain, including in the USA, despite often being highly toxic. Many are now known to act by encouraging pelvic blood flow and promoting menstruation, or to contain oxytocin, the hormone that induces contractions and labour. Although abortion is a contentious issue today, Silphion was literally worth its weight in silver in Roman times, and is believed to have been harvested to extinction.
Herbal knowledge was lost in Medieval Europe, with suggestions that governments suppressed information in order to accelerate population growth in the wake of the plague epidemics. However, condoms were already in use by that time, though the first generation were intended to prevent the spread of syphilis, which had recently emerged as a sexually transmitted disease (STD), rather than pregnancy.
Things changed in 1677 with the discovery of sperm by microscopist Antoine van Leeuwenhoek, and condoms became popular contraceptives. The infamous Venetian lover Giacomo Casanova discussed their use as birth control in his memoir, Histoire De Ma Vie. He favoured those made of lamb intestine over earlier linen varieties, but also made use of lemons as a barrier method for women, the acidity of which probably made them remarkably effective.
Early condoms were expensive and unreliable, but a breakthrough came with the development of vulcanisation, the polymerisation of rubber to make it elastic. Unfortunately these rubber condoms were still prohibitively expensive for the lower classes, and had to be kept and reused. However, the invention of Latex in the 1920s made manufacture easier and the quality better, and is still the main material used today. This centuries-old technology remains among the best methods for preventing STDs.
With an increase in sexual education and demand for birth control, there also came a rise in opposition. Condoms were attributed with a decrease in birth rate in Britain during the 17th century which led to their condemnation by the Catholic Church and a witch-hunt against midwives who promoted birth control. In the USA, the Comstock Act of 1873 placed a complete ban on contraception and many other countries followed suit.
However, by this time conception was much better understood, following the discovery of the human egg in 1827, and its fertilisation by sperm in 1843. Later came the realisation that one egg was released during each menstrual cycle, corresponding to a woman’s most fertile period. This formed the basis of the rhythm method, in which the sperm and egg are prevented from meeting by only allowing sex during the least fertile period of the menstrual cycle. Though an imperfect science, it remains the only form of contraception accepted by the Catholic Church.
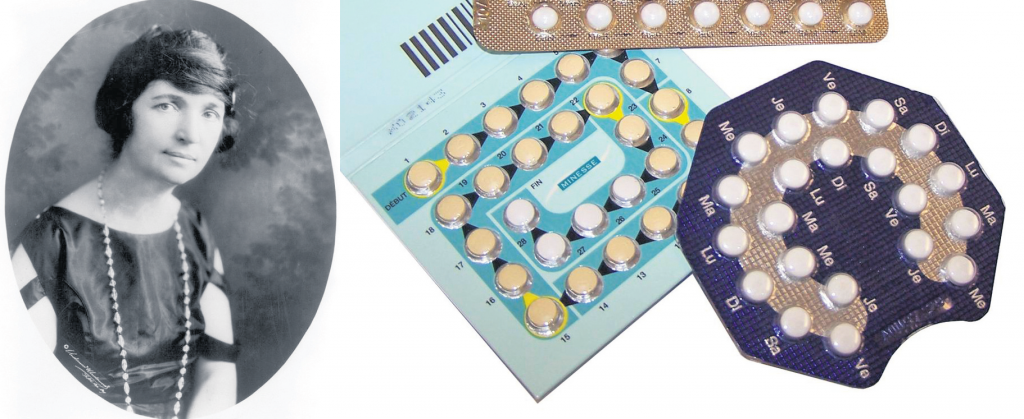
Despite this new information, the rhythm method was not deemed effective enough for a woman named Margaret Sanger. A nurse by training, she had watched her mother die from the exhaustion of carrying 18 children in the wake of the Comstock Act, and dreamt of a pill to prevent other women from suffering her mother’s fate. In the first half of the 20th century she founded, and was arrested for, the first birth control clinics in the US.
Sanger recruited scientist Gregory Pincus to work on her pill, and a Catholic physician, John Rock, who was working on hormonal treatments for infertility. Together they established that progesterone, a recently discovered female hormone, suppressed the release of an egg and, ironically for Rock, consequently prevented conception. As birth control was still illegal, their drug was marketed for ‘female disorders’ until the Food and Drug Administration approved it as a contraceptive, named Enovid, in 1960. Although initially limited by law to married women wishing to control family sizes, the Pill’s usage has since exploded. In the 2000–2010 period, World Health Organisation statistics indicated that it was used by 62 per cent of women in sexual relationships worldwide. In addition many alternative methods have arisen from the original hormonal research, including contraceptive injections and implants, and the morning after pill.
Now the focus has turned towards men, as researchers work on developing a male pill to block the hormone testosterone from stimulating sperm production. Chemicals have also been developed to physically block the release of sperm, while in work published this year, ultrasound was shown to reduce sperm counts in rats. Further research is required to establish the long-term safety and efficacy of these techniques, but new contraceptives are on the horizon.
Contraception is among mankind’s most important, but controversial, inventions. It has enabled us to manage population sizes and has been instrumental in reforming gender roles and promoting women’s rights. It has been blamed for the breakdown of marriage and societal values, and even now, people in some nations still have to fight for what the West sees as a basic human right. But controversy aside, we have found a way to overcome our most basic biological purpose, to reproduce, and for that scientific achievement alone it is worth recognition.
Vicki Moignard is a 1st year PhD student in the Department of Haematology