SUNDAY, 7 NOVEMBER 2010
Why do we get sick? The 2009 pandemic of swine flu was just another demonstration of how vulnerable we are to those minute particles known as viruses. Fortunately, the cost in human lives of this new version of the influenza virus was much lower than initially feared. However, looking back at recent human history, there has been no shortage of mass killer diseases, from the 1918 Spanish Flu to the ongoing HIV pandemic; new pathogens keep sprouting up like weeds in a garden. But why can’t we just develop an impervious immune system? Part of the reason may be that it isn’t in our best interest to do so; sometimes we can actually use viruses to our advantage.Every time we get infected with a new pathogen, our immune system not only fights it but also keeps a record of it in the form of antibodies, ensuring a swift and efficient response the next time we encounter the same microbe. In addition, because we have all inherited a slightly different immune toolkit from our parents, individuals who are better equipped to resist a new deadly disease will stand a better chance of passing on those good genes to the next generation.
Thus our species, like all living organisms on this planet, keeps evolving and adapting to an ever-changing environment. This coevolution is like an eternal arms race between host organisms and their pathogens.
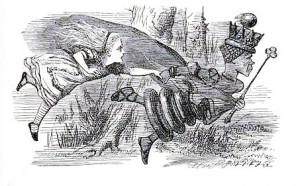
American biologist Leigh van Valen has likened this struggle to Lewis Carroll’s Red Queen Race, borrowing her famous phrase: “it takes all the running you can do, to keep in the same place.” Although this antagonistic vision of the relationship between a pathogen and its host makes intuitive sense, it is only part of the story. Natural selection may unexpectedly favour imperfect immune systems, enabling a host to maintain a pathogen and use it as a biological weapon against competitors.
Most people in England are familiar with the grey squirrels that dwell in many parks and wooded areas. A species native to North America, the grey squirrel was introduced to Britain only a century ago by travellers returning from the New World. It rapidly replaced the indigenous red squirrel, which still survives in parts of Wales, Scotland and most of continental Europe. While it had been thought for decades that the newcomers were simply better adapted to colonise our environment than their ginger-haired cousins, scientists recently discovered that grey squirrels had a microscopic ally: a virus.
A large number of red squirrels at the fringe of the red-grey divide in Northern England were found to have died of a squirrel pox infection. Meanwhile, the grey squirrels were often found to possess antibodies against that same virus, suggesting they may be healthy carriers. The current hypothesis is that the invaders have been unwittingly using the virus as a biological weapon against the red squirrels. The irony of this story is that the squirrel pox virus is a distant relative of the human smallpox virus that was introduced to the Americas by European settlers. The smallpox virus was also mostly introduced unwittingly, but at times deliberately, and it had the more horrifying effect of decimating the American Indian populations.
This tale of two squirrels is just one illustration of a widespread phenomenon termed ‘pathogen-mediated competition’. It affects a wide range of animals, plants and even microbes. Many of the bacteria that make us sick by colonising our intestinal or respiratory tracts can themselves become infected and killed by specialised viruses known as bacteriophages. However, some bacteria are capable of harbouring a dormant version of the bacteriophage that only gets activated if the host bacterium gets stressed. When that happens, copies of the virus are rapidly produced and start infecting the surrounding bacteria – except those that carry the dormant bacteriophage, which confers them immunity. Experiments have shown that this strategy (of carrying what is effectively a time bomb) can enable bacteria to invade an environment previously occupied by a competitor that has no protection against the bacteriophage.
This teaches us an important lesson about the evolution of immune systems: instead of continuously trying to wipe out pathogens, it can be more efficient to tolerate their presence and use them as weapons against competitors. As far as natural selection is concerned, it does not matter if a pathogen makes you sick as long as your competitors get even sicker. Furthermore, all organisms have to allocate a finite amount of resources into a wide range of vital functions, so increasing the investment in immune defences may have to be at the expense of another necessity. The optimal allocation of resources (i.e. the one that achieves the best reproductive success) depends on the benefits and costs associated with each vital function.
In the case of immunity, the benefits depend on the risk of getting infected and the virulence of that infection. Most infections are spread by some form of contact between conspecifics (individuals that are likely to compete among themselves for access to food, habitat or sexual partners). As a result, the risk of infection for an individual is in part dependent upon the immune defences of its competitors. If all conspecifics are well protected, they are unlikely to harbour and transmit infectious agents. So, even if you do not invest much in your immune system, you may still be protected by your neighbours, as long as they are ready to pay the cost. This indirect protection is known as ‘herd immunity’ and is an essential factor in the spread of disease.
Herd immunity presents an evolutionary conundrum: if the cost of immune defences is paid by the individual but its benefits are shared with neighbours through herd immunity, no one is expected to evolve a strong immune system. Natural selection appears to favour investing a minimum amount of resources in the immune system while taking as much advantage as possible of the investments of others. So does that mean we cannot hope to win the war against pathogens? Actually, if those pathogens can be used as biological weapons against competitors who are more susceptible to infection, we may not want to kill all our microbial enemies. Instead, it can pay to learn to live with them.
Olivier Restif is a postdoc in the Department of Veterinary Medicine