FRIDAY, 25 JANUARY 2013
Despite being a theme in many works of science fiction, metamorphosis (from the Greek meta “change” and morphe “form”) is hard to find in any human biology textbook. We are all familiar with the notion of a caterpillar transforming into a butterfly, but we firmly agree that similar kinds of wizardries are peculiar to (or a peculiarity of ) bizarre insects, exotic fishes and monstrous super heroes. While this holds true for the normal life cycle of a human being, recent advances in the fields of stem cells and developmental biology suggest that we are far less unchangeable than we previously realized.It is well known that the many hundreds of different cell types that provide the building blocks of our body all possess identical genetic material. Unsettling as it was at the time of its discovery, this apparent paradox has been eventually reconciled by the strenuous work of two generations of geneticists. Over time, geneticists have proven that tight regulation in the expression of our genetic code is the key to the many observable differences in cell identity and specialisation. A vast array of proteins silently pulls the strings of our cellular destiny by interacting with our DNA, sculpting its structure in order to “hide” the undesired pieces of genetic information. As cells progress from the primitive state of the early embryo through the different stages of development, this process gradually defines the different colours, shades and tints of our cellular palette, by gradually restricting the expression of genetic traits down to the minimum required for each specific cell function.
This elegant hierarchical model implies that each cell gradually loses its ability to become many different kinds of cell by choosing to proceed down a particular branch of development at each crossroad of the cell-fate highway. However, as for every good rule there have to be some exceptions. Curiously enough, the first and more notable of such incongruities was observed even before the establishment of the model itself, when John Gurdon completed the first successful cloning experiment. He showed in 1962 that the fate of an otherwise lifeless, immature tadpole egg whose nucleus had been removed could be rescued by implanting the foreign nucleus of a mature frog cell, thus artificially creating life. The profound implication of this experiment was that the genetic information previously “hidden” in the mature donor could be successfully utilised by the DNA-deficient tadpole egg, showing that the status of the adult cell is not irreversible. More recently, this notion was further expanded by the work of Shinya Yamanaka, who showed how a similar “reprogramming” of adult cells to a primitive state can be achieved by exposing a cell to a cocktail of only four proteins . Notably, Gurdon and Yamanaka were recently awarded the Nobel Prize for Physiology and Medicine 2012, an acknowledgement of the tremendous impact of their discoveries.
While Yamanaka’s work has established the current paradigm of cell-fate manipulation by the use of only a few defined factors, there are many other less famous examples of similar processes. As many as eighteen years before Yamanaka’s breakthrough, the pioneering work of Andrew Lassar proved that the expression of a single protein called MyoD was able to transform cultured human skin cells into muscle — a process which we could call “metamorphosis”. More recently, fuelled by the hopes raised by previous studies, an army of scientists rushed towards the discovery of a medical philosopher’s stone, the ability to convert skin cells into clinically-desirable cell types. Unlike their ancient counterparts, these modern alchemists were successful in their attempts, and the metamorphosis of skin into blood, liver, pancreas, brain and heart is no longer a fantasy of science fiction writers.
The discovery of cell-fate manipulation is certainly Nobel Prize winning, but does it have any practical uses beyond the creation of frogs and Frankenstein? The answer is unequivocally yes with applications extending throughout the medical and biological community. Firstly, cell transformation allows scientists to create experimental tissues in which to study human diseases, thus circumventing the difficult task of acquiring precious samples from human donors. In addition, these same cells could be transplanted into patients to regenerate damaged tissues, with scientists currently investigating the possibility of introducing insulin-producing cells into the pancreas of diabetics and neurons into the brains of Parkinson patients. Finally, an even more ambitious approach would be to instruct the cells of our own body to transform into a desired tissue which needed to be regenerated. This would bypass the need to isolate and cultivate the cells in a laboratory, thus dramatically reducing timing, costs and impact on the patient.
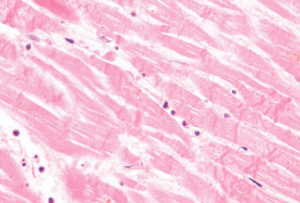
Despite sounding like the plot of a science fiction movie, this kind of medical treatment might be closer than we would have ever dreamed. Earlier this year two separate studies independently reported the successful in vivo reprogramming of cardiac non-muscle cells into contractile tissue. After a heart attack, the heart muscle which suffered from a prolonged lack of oxygen dies and is substituted by cells of the connective tissue. These cells form a scar. This mechanism preserves heart function over the short term, but eventually leads to dysfunction as the scar is not able to contract, which imposes an increased burden on the rest of the muscle. This situation gradually evolves into heart failure, as the oxygen supply to peripheral organs becomes insufficient. Unfortunately, this is relatively common in Western countries, and a heart transplant is the only radical solution to the problem. Any development which aims at regenerating the damaged muscle in the early phases after a heart attack would be very useful. Deepak Srivastava and Eric Olson’s research groups believed that if they could make the cells in the scar “transform” and become tissue that could contract, then the lifespan of the heart after a heart attack would be increased. To this aim, they genetically engineered some modified (noninfectious) viruses in order to carry the genetic information required for the expression of some “muscle-transforming” proteins, and they injected them into the affected areas of the hearts of mice. Strikingly, not only did they observe some degree of transformation of scar cells into contractile muscle tissue, but this was sufficient to reduce the cardiac dysfunction in the mice.
Is this the dawn of a new generation of regenerative medicine-based treatment? Is this the first step towards reaching human immortality? Scientists predict that this technology will make the leap from laboratory bench to patient’s bedside in the next few decades, but stress that we can probably answer yes to the first question but add that even the most optimistic estimates for this kind of treatment to reach patients cannot be shorter than ten or twenty years. Much more research will be needed before we can properly understand and control cellular reprogramming in a safe and efficient way. As for human immortality, we can leave it to the words of the famous science fiction novelist Arthur C. Clarke: “The only way of discovering the limits of the possible is to venture a little way past them into the impossible”.
Alessandro Bertero is a 1st year PhD student in the Department of Surgery