WEDNESDAY, 15 MAY 2013
We stand on the brink of the post-antibiotic era, with bacteria becoming increasingly resistant to existing drugs and with few new ones in the pipeline. In light of this fact, scientists are revisiting early antibiotic agents in the search for a new wonder drug with which to tackle the escalating bacterial threat. One of the most common groups of antibiotics, penicillin, only became widely available during World War II, with one of its first high profile uses taking place in the aftermath of the D-Day landings. However, researchers had first highlighted bacteria as a cause of disease about 70 years beforehand. Indeed, the history of antibiotics prior to the popularised use of penicillin is incredibly rich with attempts to find the ‘magic bullet’ against infection. Reconsideration of this early research may offer the solution to this looming medical dilemma.In 1877, Louis Pasteur and Jules Joubert developed the concept of antibiosis, a process in which one microbial species attacks another. This was not the first description of antibiosis, however. John Tyndall had previously reported the lysis, that is the destruction of a cell by rupture of the cell wall, of bacteria in the presence of a Penicillium mould. Nevertheless, the report by Pasteur and Joubert can be considered one of the first appearances of antibiosis in literature that survives modern scrutiny, and certainly one of the most widely disseminated pieces. By 1885, Victor Babes had shown that it was chemical substances produced by microorganisms that killed bacterial species. In that same year, Arnaldo Cantani carried out one of the first recorded therapies based on antibiosis, treating a patient suffering from tuberculosis with a Bacterium termo culture, applied directly into the lungs of the patient. The tuberculosis bacteria disappeared from the patient’s mucus, replaced by B. termo, and the patient’s condition improved. Many more cases involving the replacement of pathogenic bacteria with less harmful ones were published in scientific literature in the following decades.
Other early applications of antibiotic treatment included the use of microorganism-derived lytic substances in the preparation of vaccines. However, these injected chemical agents were not truly chemotherapeutic because they did not effectively treat infection and disease—they could only prevent them. Several scientists attempted to develop chemotherapeutic agents, and one such product, pyocyanase, became the first to be distributed to hospitals. Discovered independently by Ivan Honl and Jaroslav Burkovsky in 1898 and by Rudolph Emmerich and Oscar Löw in 1899, it was released by the latter after they observed its lytic effects against many bacteria, including those causing cholera, anthrax, typhoid and plague. Whilst they were unsure of its origin or mechanism of action, it proved bactericidal and effective in the clinic. After several years, it had become primarily used as a local antiseptic to great effect, successfully treating a wide variety of cases ranging from diphtheria to conjunctivitis. However, by the late 1920s it had fallen out of clinical use due to inadequate quality controls in production, resulting in an inactive product and a subsequent loss in sales.
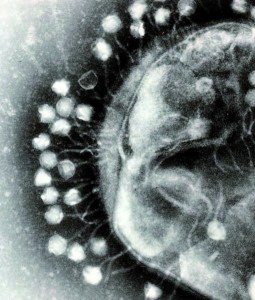
Another group of pre-penicillin chemotherapeutic agents comes from an unlikely source: a group of viruses known as bacteriophages, which solely infect bacteria and are often species-specific. Although Frederick Twort and Félix d’Herelle independently discovered bacteriophages in 1915 and 1917, respectively, it is d’Herelle that stands out as the father of bacteriophage therapy and indeed remained one of its most vocal proponents throughout his life. Realising that commercial laboratories were producing inactive preparations due to poor quality controls, drawing much comparison with pyocyanase, he established his own laboratory to research, produce and distribute phage products in an effort to prevent their discredit. He travelled extensively to introduce phage treatment around the world, and it is largely due to his efforts that it maintained a strong presence in France until the 1990s and is still widespread in Eastern Europe today. Indeed, in the brief conflict between Russia and Georgia in 2008, Georgian soldiers were deployed with phage cocktails amongst their medical supplies. What makes phage therapy most interesting in the pre- penicillin context is that no one at this time was quite sure what phages actually were, lacking the technology to visualise these viruses.
One of the last major groups of antibacterial drugs to experience a phase of strong popularity was the sulphonamides, first popularised in a prodrug form trade-named Prontosil. Prodrugs are biologically inactive compounds that are converted into their active form in the body by normal metabolic processes. Although initially patented by the German company IG Farben that first demonstrated its medical potential, the active component was later found to be a sulphonamide on which the patent had long since expired. It enjoyed a brief moment of pharmaceutical dominance in the late 1930s and was available both in a pill and powder form. Unfortunately, it was ineffective in pus-infected wounds and therefore had limited success in treating established infections. Its derivatives are still in use today, most notably in the dual content drug Trimethoprim/sulfamethoxazole (TMP/SMX). Another noteworthy drug is the chemotherapeutic agent Salvarsan (later replaced with Neosalvarsan), discovered by Paul Ehrlich’s laboratory in 1909. A product with a niche market, it was only effective against syphilis and remained popular in clinics until eventually superseded by penicillin.
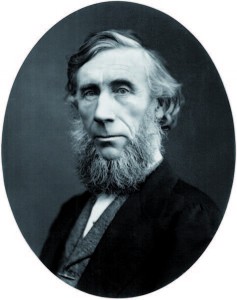
Finally, the history of penicillin itself is not as straightforward as is often believed. As mentioned above, John Tyndall noted its antibiotic effects in 1875, while Joseph Lister, who in 1871 apparently used penicillin to treat a patient, and Louis Pasteur reported similar observations in the same decade. The physician Ernest Duchesne also carried out key work in 1897, and his doctoral thesis on Penicillium glaucum described the mould’s use in successfully treating typhoid in guinea pigs. However, we now know that penicillin is inactive against typhoid and so it seems likely that he misidentified the mould, perhaps confusing it with a member of the genus Acremonium, a group that produces cephalosporins—a family of chemotherapeutic agents active, among others, against typhoid. Ultimately, the work was largely ignored, most likely due to Duchesne’s lack of scientific seniority.
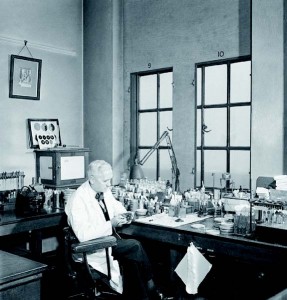
It was not until 1928 that Alexander Fleming first published work on penicillin, also largely disregarded at the time, and by 1935 at the latest he had all but abandoned his work on penicillin, focusing his interest on the newly discovered sulphonamides. Others attempted work with the unstable mixture, most notably Harold Raistrick, Percival Clutterbuck and Reginald Lovell, but while they found they could biochemically purify it, they were ultimately unable to extract it from solvent. It was not until scientists such as Howard Florey, Ernst Chain and Norman Heatley at the Dunn School of Pathology, Oxford took up the task of isolating and stabilising penicillin that its large-scale production was possible, thus helping to introduce the antibiotic era.
The road to readily available and safe antibiotics was one filled with many promising compounds and many others that resulted in dead ends. Poor quality controls, temperamental products and a lack of recognition by the scientific community were all factors responsible for the lack of long-term uptake of pre-penicillin antibiotics. Meanwhile, penicillin’s remarkably low toxicity and ease of application allowed it to dominate the antibiotic market. If and when we enter the post-antibiotic era, it will be vital to promptly establish alternative forms of treatment, and it may well be that some of these early therapies make a comeback.
Nathan Smith is a 1st year undergraduate studying Biological Natural Sciences at Churchill College