TUESDAY, 20 MAY 2014
The term ‘stem cells’ has become one of the most widely-used scientific expressions of our time, and the extreme popularity of stem cells in the media has established them as a part of modern culture. As a result, everyone seems to know what a stem cell is, and what a stem cell can do. Nevertheless, some clarification can be of particular use in this case, as the social and political implications of stem cell use are growing increasingly complicated.A stem cell has the potential to divide itself indefinitely and to differentiate into any specialized cell type. Over the last few decades, researchers have discovered many types of human stem cells that can be found throughout development and adult life. Theoretically, cultivation and differentiation of stem cells under specific conditions in laboratory settings offer the chance to generate nearly unlimited copies of any cell type of the human body, hence presenting the possibility of replacing faulty or deceased cells with healthy ones. However, the leap from acknowledging these opportunities to believing that humankind had found a long-life elixir was, for the media and the public, unrealistically short.
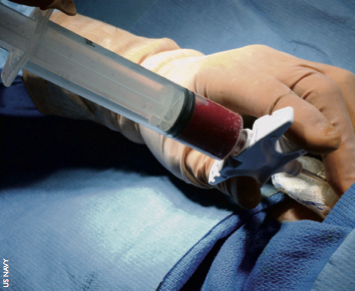
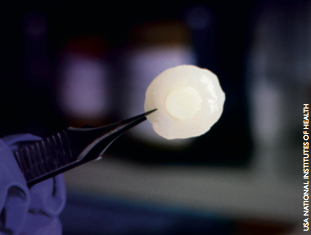
Overwhelming coverage in the media has led the public to believe that in the near future, terrible diseases like Alzheimer’s, cardiac failure and diabetes will be cured. However, several years down the line, the hype of stem cell therapies has proven to be excessive. In fact, most stem cell based cures are still going through laboratory and clinical evaluation, with the exception of a few notable applications in corneal, skin and bone marrow replacement.
Given the complexity involved in developing such therapies, this delay may be unsurprising to most scientists, but is having dangerous effects on the wider public.
Private clinics around the globe have been instilling false hope in a growing number of patients, promising miraculous stem cell based cures. Instead of losing faith in the clinical applications of stem cells, more and more people have started to look for these therapies outside the evidence-based medicine, in particular victims of devastating diseases for which ‘conventional’ medical practice provides no definitive treatment. These controversial ‘therapies’ are most notably offered in India, Japan, China, Mexico and Costa Rica, in which the regulation for the use of stem cells is very loose, often allowing unaccredited laboratories to offer putative treatments for autoimmune, neurological, metabolic and even genetic disorders. The resulting predicament has been described as ‘stem cell tourism’, and its social and medical complications are growing. Well- documented cases of patients getting severely worse vastly outnumber the few sporadic and dubious reports of miraculous outcomes.
This phenomenon reflects the general public’s deep ignorance of stem cell research, and it is the people responsible for educating and protecting patients who are to blame. Scientists, journalists and governments have all contributed to this misinformation by failing to accurately communicate the reality and limitations of stem cell technology. This is one of several examples of modern scientific discoveries, in which the will to justify huge public research investments has overshadowed the need for accurate scientific divulgation. Indeed, a similar situation occurred when the human genome was first sequenced in 2001. This crucial milestone was welcomed by premature claims of having found the key to cure all human diseases, but after more than a decade of research, we are still unable to fully understand most of the information encoded in our DNA.
More recently, the confusion between the fact and fiction of stem cell therapy has resulted in multiple private companies and lobbyists trying to bring the flux of ‘stem cell tourists’ back to the US and Europe, by attempting to subvert local regulation regarding stem cell use. An emblematic case happened in Texas in 2011, when Governor Rick Perry supported the loosening of stem cell legislation. By categorising stem cell therapies as tissue transplants instead of biological drugs, the new state rules allowed several companies to bypass the federal law requirement for clinical trials before treating patients. Perry himself became the first patient of one of these companies, Celltex, and was hence accused of having a conflict of interest, despite not being a shareholder. The new regulation led to a legal dispute that eventually halted most of these procedures and stirred a polarising public debate, where the understandable emotional considerations of patients claiming their right to decide their own treatment quickly overwhelmed legal and scientific arguments.
A very similar scenario is happening in Italy, where the so-called ‘Stamina method’ is dividing public opinion. The procedure has been repeatedly stopped due to growing concerns regarding its safety, methodology and therapeutic rationale, but then re-authorised by sentences from local courts, backing ferocious public protests that claim the right of patients to be treated.
Apart from providing more evidence that better communication of facts in stem cell research is mandatory, these cases also reflect another controversy in the field. For the first time, public attention is being drawn to the scientific and legal debate on how stem cell therapies should be regulated. A growing number of scientists are starting to believe that the current legislation might not be completely appropriate. For example, some claim that rules originally established for chemical drugs do not take into account the intrinsic differences between normal medication and stem cells. The dilemma of complying with the strict normative guidelines of the so-called ‘Good Manufacturing Practice’ when dealing with stem cells is regarded by some as a major obstacle in the development of novel therapies. Moreover, it is important to realise that pre-clinical studies of efficacy in animal models might be particularly inappropriate when studying human stem cells. Another opposing argument is that clinical trials with stem cells are often approved only in patients that are in a very late stage of illness. This reduces the chances of a therapy to show efficacy (it can be argued that many of the now established stem cell therapies would not have been approved within the current legislation) and prevents other patients from accessing such trials because they are, paradoxically, ‘too healthy’.
Legislation itself has also been blamed for the rising rate of ‘stem cell tourists’. Some people argue that patients are getting so frustrated with the lack of access to ‘canonical’ stem cell clinical trials that they turn to other stem cell sources. Even from a neutral standpoint, it is clear that proposed changes in stem cell legislation should not be considered taboo; they should be carefully and logically evaluated for pros and cons, as well as applicability and feasibility.
It is rare for fields in medicine and science to reach such a level of publicity and controversy as stem cell therapy has received. With many therapeutic milestones already achieved, and several others in close reach, stem cell technology presents one of the greatest opportunities for humanity to eventually treat numerous devastating diseases. However, as with any great power, the use of stem cells comes with great responsibility. It is now apparent that the path towards the safe therapeutic application of stem cells is a tightrope-walk rather than a downhill-race. Indeed, we must inform public opinion about the scientific facts of stem cells, as well as scrupulously maximise the potential of this technology while carefully protecting patients. The prize is big, as are the potential pitfalls–the game is on.
Alessandro Bertero is a 2nd year PhD student at the Department of Surgery