THURSDAY, 1 APRIL 2021
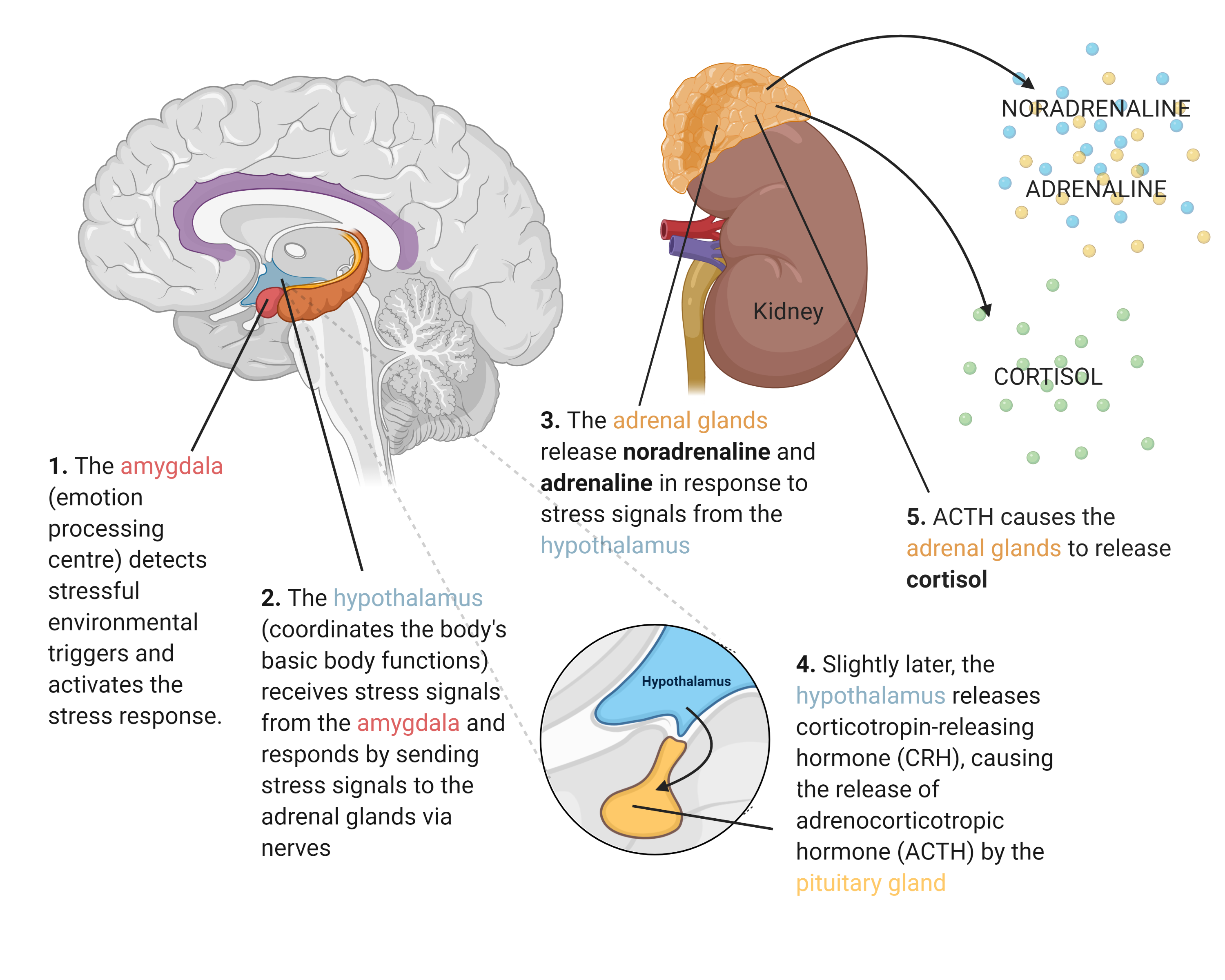
Stress is an unavoidable part of life. For something so draining, most people never imagine that those days of exam cramming or worrying about family might lead to long-lasting health consequences. At most, you might have noticed the pimples that seem to come up before that tight deadline, or the colds you come down with just after. Recently, however, the scientific world has begun to realise that, as abstract as psychological stress may be, it can have a very concrete influence on our physiology and the illnesses we may be at risk from. In particular, stress is thought to reprogram the immune system, increasing susceptibility to immune-related illnesses.What chemical changes accompany those unpleasant feelings of psychological stress? Stressful environmental triggers will activate a variety of brain centres that then mount a hormonal stress response, during which stress hormones are released from the adrenal glands. This process occurs in two stages. In the first stage, noradrenaline and adrenaline are released, hormones that mediate the ‘fight-or-flight’ symptoms of stress, such as an increased heart rate. In the second, cortisol is released, a hormone that ensures the continued maintenance of the stress response.
Noradrenaline, adrenaline, and cortisol exert their effects by binding their respective receptors on nearly all cells of the body. Binding leads to changes within the cell that prepares the body for a ‘fight-or-flight’ situation. Within the immune system, this leads to the activation and redistribution of immune cells from the lymph nodes into the bloodstream and to vulnerable areas such as the skin. This process is known as inflammation and helps prepare the body to fight potential infections, which may accompany the stressful environmental trigger. More specifically, noradrenaline and adrenaline stimulate inflammation, while cortisol has a more regulatory effect, helping to keep this inflammation from getting out of control and becoming damaging.
This acute change in the immune system in response to stress is generally useful, protecting the body against infection in potentially dangerous situations. The issue arises when this stress response is chronically activated, as it is in certain stress-related conditions such as generalised anxiety disorder, or in long-term suffering. It is hypothesised that chronically elevated cortisol levels can lead to cortisol resistance — where the same level of cortisol no longer exerts an effective regulatory response. Subsequently, chronic inflammation ensues, where the pro-inflammatory effects of elevated noradrenaline and adrenaline are no longer controlled.
Chronic Inflammation Can Only Be Bad News | Chronic inflammation underlies a range of seemingly unrelated illnesses. The ability of psychological stress to induce and exacerbate this condition means that it is a serious health risk which is only beginning to be taken seriously. For example, chronic psychological stress has been observed to increase susceptibility to certain infections. Initial work has suggested that infection rates of the common cold were higher in individuals exposed to higher levels of psychological stress. Recent work has also indicated that individuals with stress-related disorders such as anxiety or PTSD are at a higher risk of contracting life-threatening infections. This association was mainly observed for infections which involve some kind of overreaction of the immune system, indicating that chronic inflammation could be the underlying connection between the two factors. This is extremely applicable to the ongoing COVID-19 pandemic, where researchers are looking for reasons why some patients experience severe immune overreaction in response to the virus, leading to serious disease. Early work on COVID-19 has already observed strong associations between stress-related mental illness and COVID-19 severity.
Chronic stress has also been associated with incidence of autoimmune disorders. A 2018 study concluded that having a clinical diagnosis of a stress-related disorder significantly increases the risk of autoimmune disease in later life. This is consistent with previous work that has associated chronic stress with flare-ups and incidence of rheumatoid arthritis, multiple sclerosis, Crohn’s disease, type I diabetes, and several other autoimmune diseases. Mechanisms behind this link are still unclear but initial studies in chronically stressed children indicate pro-inflammatory responses to self-proteins, consistent with cortisol insensitivity. Chronic inflammation induced by chronic stress is therefore a probable explanation, although more complicated imbalances in immune cell profiles are likely to be involved in this complex process. This is also likely to underlie the association between chronic stress and other immune disorders. Maternal stress during pregnancy, for example, has been observed to increase rates of asthma and dermatitis, both allergic conditions caused by hyperinflammation. Links have even been established between stress, chronic inflammation, and Alzheimer’s disease, which is recently beginning to be considered an immune disorder.
Stress-induced chronic inflammation is also thought to be a predisposing factor for mental health disorders. Stress-induced neuroinflammation in glial cells, which surround and support neurons in the brain, can disturb the production of neurotransmitters such as serotonin, melatonin, or glutamate. The imbalance of these key hormones can predispose the individual to mental health disorders. This effect has been observed in the manifestation of anxiety, depression, PTSD, and schizophrenia. It has also been supported by studies where chronic inflammation induced by chronic stress in rats correlated with an increase in depressive and anxious behaviour. It is commonly accepted that periods of stress and personal suffering can often lead to mental health issues such as depression or anxiety; by looking at the link between chronic stress and the immune system, concrete mechanisms for why exactly this occurs are beginning to emerge.
Why Does Any of This Matter? | Psychological stress has largely been ignored in the quest for new therapeutics; more traditionally physiologically important processes such as heart function or cell cycle regulation tend to take priority in medical research. The abundance of new evidence connecting chronic stress to immune-related illness now begs to differ — psychological stress must be taken just as seriously. With the advancement in knowledge of how stress drives disease, we can create drugs to reduce the risk of those with mental health issues developing life-threatening illnesses, or to mitigate the suffering of people with stress-induced disorders.
Of course, there are still many barriers preventing true progress in this field. Stress is often accompanied by physiologically damaging behaviours such as smoking, worsening sleep patterns, or increased drug use. It is often difficult to separate the effects of these behaviours from those of stress itself. Scientifically robust experiments are also difficult to conduct, as stress is very personal, and is defined differently for each individual. The immune system is also vastly complicated, and the true interaction between chronic stress and immune dysregulation is far more complex than the simple mechanisms described here. This complexity will take a large amount of time to be unravelled.
Despite this, the connection between psychological stress and the immune system is undoubtedly an exciting avenue for future research. The conditions mentioned here only skim the surface of diseases that may be connected to stress via inflammation — obesity, ageing, and cancer are also known to be involved, to name just a few. Perhaps the lesson here is to respect stress just that little bit more. Next time you notice that stress pimple or cold, stop and rest, just like you would with any other illness — it may be doing more damage than you realise!
Eleanor Sherlock is a 3rd year Natural Sciences Undergraduate at Magdelene College. Artwork by Biliana Tchavdarova Todorova.
